The Longevity Shift: From Reactive Medicine to Proactive Healthspan
You may also like :
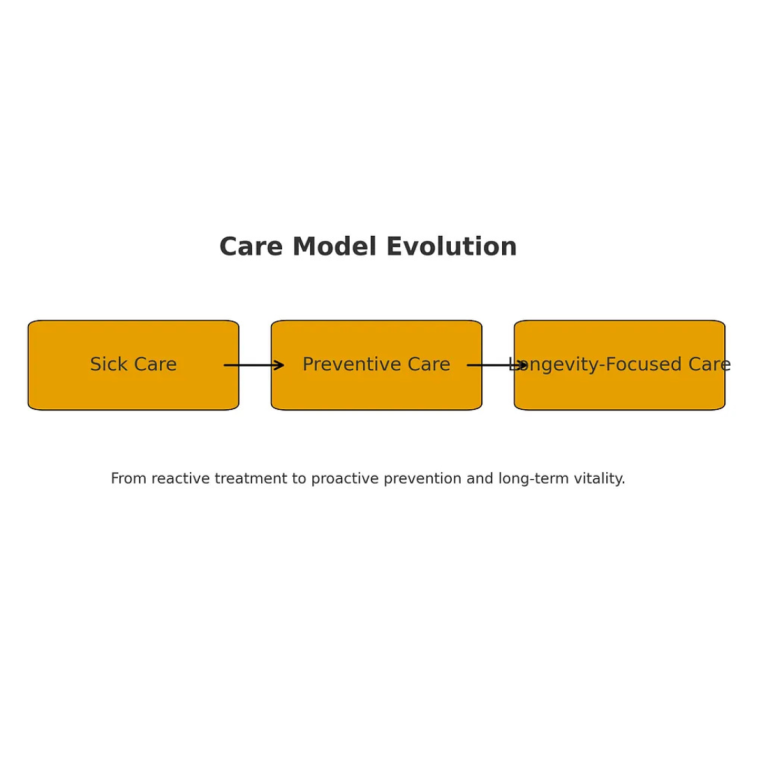
We’re at a tipping point. For decades, our healthcare system has been built around diagnosing and treating disease once it appears, chronic conditions, acute episodes, hospitalization, rinse and repeat. But now a new paradigm is emerging, one focused on extending healthspan, not just lifespan, on monitoring biology, not waiting for illness, on enabling doctors and patients to work together early rather than playing catch-up later.
In recent years, clinics with a “longevity” mindset have started proliferating. These practices offer more than a 15-minute annual check-up. They deliver deep diagnostics, including genetic and epigenetic testing, metabolic profiling, microbiome analyses, detailed imaging, wearable integration, and then assemble personalized intervention plans around those insights.
But the shift raises two big questions:
1. Will this model move from early-adopter luxury to broad access?
2. What role will the many companies supporting this shift play, startup disruptors, technology platforms, and those building infrastructure?
Below, I’ll walk through the current state of longevity clinics, the access challenge, and how Dapper is positioning itself amidst this mix.
⸻
What Today’s Longevity Clinics Look Like
The longevity clinics of today aim to deliver health diagnostics and optimization that sit far beyond traditional primary care. In some cases they are replacing primary care altogether for a subset of well-resourced patients.
Common features include:
• Multi-hour intake visits rather than five-minute check-ins, full body MRI, advanced blood panels including biomarkers of aging, DNA methylation clocks, microbiome, metabolic and cardiovascular imaging.
• Integration of wearables and continuous monitoring into the care plan, so that sleep patterns, activity, heart rate variability, glucose or other markers feed into real-time feedback loops.
• Personalized lifestyle and therapeutic interventions such as diet, exercise, sleep, stress resilience, and sometimes regenerative medicine approaches including stem cells and peptide therapies, although with varying evidence.
• A shift in mindset, aging considered not only as something to accept but as a process that can, in principle, be slowed, managed, or optimised.
“Growing older does not have to mean slowing down. It means getting smarter about how we age.”
In short, instead of waiting for disease, the idea is to intercept biology before disease manifests.
⸻
The Access Problem: Why It’s Not Yet for Everyone
Despite the promise, there are clear headwinds:
1. Cost and affordability. Many of these clinics charge luxury-tier membership or intervention fees, often not covered by insurance. Some packages run into tens of thousands of dollars annually.
2. Scale and infrastructure. Standardising diagnostics, managing large data flows, and integrating with EMRs and outcomes tracking remain challenging. A recent survey found that only about 40 percent of longevity clinics were fully integrated with health records, and formal training programmes for longevity providers are still patchy.
3. Evidence base and regulation. While many interventions are scientifically promising, ageing is complex and heterogeneous. The field is still building consensus on biomarkers, validated endpoints, and long-term outcomes.
4. Equity and scale. Right now the model favours affluent, health-primed individuals. Without new models or cost innovations, the longevity revolution risks becoming a niche for the few.
“The longevity revolution cannot just belong to the wealthy. Access is the real frontier.”
The vision is exciting, but the business and operational model is still maturing.
⸻
Where Platforms and Startups Come In
There is a growing ecosystem of companies building the durable infrastructure for this longevity-centric medicine. These firms provide diagnostics, analytics, monitoring tools, pharmacy and compounding workflows, AI engagement engines, and physician-support platforms.
One such company is Dapper, which I lead. Although our immediate model isn’t exclusively marketed as a “longevity clinic,” the capabilities we are building map directly to the longevity agenda.
For example:
• We enable physicians to deliver personalised medication fulfilment, advanced diagnostics, and wearable-data integration, while keeping the doctor at the centre of care.
• Our platform emphasises automation, adherence tracking, patient engagement, and cost-efficiency, all critical levers if longevity services are going to move beyond high-net-worth early adopters.
• We are working on solutions that support scaling so that cost per patient falls as volume rises, which in turn supports broader access.
In this way, Dapper represents one piece of the broader longevity ecosystem, the operational backbone supporting physicians who want to participate in healthspan-oriented care models.
⸻
Dapper’s AI Health Companion: Expanding Access and Supporting Physicians
Alongside these capabilities, Dapper is developing an AI health companion that strengthens both sides of the care experience.
For patients, it delivers real-time insights, symptom support, reminders, education, and personalized health guidance that helps them stay engaged long after the appointment ends.
For physicians, it reduces workload by automating routine communication, monitoring trends, highlighting concerns, and providing visibility into how a patient is progressing day-to-day.
This combination, clinical oversight paired with continuous AI support, creates a scalable path for longevity-style care without requiring massive clinic staffing or boutique pricing.
⸻
What Needs to Happen for Longevity Care to Become Widely Accessible
For this field to shift from boutique to mainstream, several strategic shifts must happen:
• Cost reduction through scale and technology. As diagnostics get cheaper, wearables proliferate, and AI automates routine monitoring, the cost of delivering longevity-oriented care must drop.
• Integration with standard health systems. Longevity models cannot sit apart. Ideally they integrate with primary care, specialists, pharmacies, and digital platforms so that the patient experience is seamless.
• Robust outcome measurement and incentives. Payers and providers will need credible evidence showing return on investment in terms of healthy years, reduced hospitalisations or disease onset, and improved quality of life. Economic modeling is promising, with studies estimating significant healthcare cost savings if biological ageing can be modified.
• Training, accreditation, and standardisation. Establishing recognised training for longevity medicine practitioners, operational standards for clinics, and ethical frameworks around emerging therapies.
• Inclusive design. Care models must account for under-served populations, not just early adopters, or the risk is a two-tier health system.
⸻
Looking Ahead: The Next 5 Years
Here is what I expect, given current signals:
- • By 2030, we will see mid-tier longevity clinics offering “healthspan tuning” for a broad adult population, not just the ultra-wealthy.
• Platform companies such as Dapper will increasingly plug into health systems and physician networks rather than trying to replace them, because physician buy-in matters.
• Diagnostics will shift from one-time snapshots to continuous monitoring through wearables and biomarkers with real-time feedback loops.
• The business model will shift. Instead of highly paid annual memberships only, we’ll see outcome-based contracts, subscription models, and bundled payments tied to health gains.
• The discussion will shift from “How long can I live?” to “How many healthy years can I gain, and how well do I live them?”
Healthspan will matter more than lifespan. The next decade belongs to preventive medicine.”
⸻
Final Thought
The longevity movement is more than a trend. It is a re-framing of medicine from reactive to proactive. As someone who lives and breathes health-tech, I believe we are entering an era where health optimisation becomes a default pillar of care, not a luxury add-on.
At Dapper, we are building the connective tissue between physician-led care, diagnostics, patient engagement, and fulfilment. And yes, while I spend a lot of time with my family and coach my kids’ Little League teams, I am also working to ensure that they get more than just years. They get quality, vitality, and choice.
Growing older does not have to mean slowing down. It means getting smarter about how we age. And for those of us who build the tools behind the scenes, it means shifting the system so that healthspan is front-of-mind for every patient.
Your Turn:
If you’re a healthcare founder, clinician, or Healthtech investor, what part of the longevity stack are you focusing on? Drop me a note. Let’s build the future together.
About the Author:
David Pachkofsky is the Founder & CEO of Dapper, a physician-focused health technology company building AI-powered tools that support long-term vitality and proactive care. Serial entrepreneur, advisor, and angel investor. Passionate about healthspan, AI, and building tools that improve people’s lives.